Comprehensive Care
The Pediatric Center has a dedicated team of 5 Pediatricians and 4 Nurse Practitioners committed to providing exceptional care for your children.
Asthma Attack
See More Appropriate Topic (instead of this one):
- If NOT, try one of these: Wheezing Other Than Asthma
Is this your child’s symptom
- Your child is having an asthma attack
- Use this guide only if a doctor has told you your child has asthma
Symptoms of Asthma
- Symptoms of an asthma attack are wheezing, a cough, tight chest, and trouble breathing.
- Wheezing is the classic symptom. Wheezing is a high-pitched whistling or purring sound. You can hear it best when your child is breathing out.
- The diagnosis of asthma requires attacks of wheezing that recur. The diagnosis is rarely made before 1 year of age.
Causes Triggers of Asthma Attacks
- Infections that affect breathing like colds or the flu
- Pollens trees, grass and weeds
- Animals like cats or rabbits
- Tobacco smoke
- Irritants such as smog, car exhaust, menthol vapors, barns, dirty basement
- Food Allergy Serious. Asthma attacks caused by food allergy can be life-threatening anaphylaxis. Examples are nuts or fish.
Asthma Attack Scale
- Mild: No Shortness of Breath SOB at rest. Mild SOB with walking. Can talk normally. Speaks in sentences. Can lay down flat. Wheezes not heard or mild. Green Zone: Peak Flow Rate 80-100% of normal rate
- Moderate: SOB at rest. Speaks in phrases. Wants to sit can’t lay down flat. Wheezing can be heard. Retractions are present ribs pull in with each breath. Yellow Zone: Peak Flow Rate 50-80% of normal rate
- Severe: Severe SOB at rest. Speaks in single words. Struggling to breathe. Wheezing may be loud. Rarely, wheezing is absent due to poor air movement. Retractions may be severe. Red Zone: Peak Flow Rate less than 50% of normal rate
- Peak Flow Meter: A peak flow meter measures Peak Flow Rates PFR. It tells us how well a person can move air out of the lungs. A PFR can be used in children 6 years and older.
When to Call Us for Asthma Attack
Call 911 Now
- Wheezing and life-threatening allergic reaction to similar substance in the past
- Starts to wheeze suddenly after bee sting, taking a new medicine, or allergic food
- Severe trouble breathing struggling for each breath, can barely speak or cry
- Passed out
- Lips or face are bluish when not coughing
- You think your child has a life-threatening emergency
Call Doctor Now or Go to ER
- Lips or face have turned bluish during coughing
- Ribs are pulling in with each breath retractions
- Peak flow rate 50-80% of normal rate after using neb or inhaler Yellow Zone
- Wheezing not gone 20 minutes after using neb or inhaler
- Nonstop coughing not improved after using neb or inhaler
- Severe chest pain
- Need to use asthma medicine neb or inhaler more often than every 4 hours
- Fever over 104° F 40° C
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Mild wheezing lasts over 24 hours on neb or inhaler treatments
- Sinus pain not just congestion
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Don’t have written asthma action plan from your doctor
- Use an inhaler, but don’t have a spacer
- Miss more than 1 day of school per month for asthma
- Asthma limits exercise or sports
- Asthma attacks wake child up from sleep
- Use more than 1 inhaler per month
- No asthma check-up in over 1 year
- You have other questions or concerns
Self Care at Home
- Mild asthma attack
Care Advice for Asthma Attack
- What You Should Know About Asthma:
- Over 10% of children have asthma.
- Your child’s asthma can flare up at any time.
- When you are away from your home, always take your child’s medicines with you.
- The sooner you start treatment, the faster your child will feel better.
- Here is some care advice that should help.
- Asthma Quick-Relief Medicine:
- Your child’s quick-relief rescue medicine is albuterol or xopenex.
- Start it at the first sign of any wheezing, shortness of breath or hard coughing.
- Give by inhaler with a spacer 2 puffs each time or use a neb machine.
- Repeat it every 4 hours if your child is having any asthma symptoms.
- Never give it more often than 4 hours without talking with your child’s doctor.
- Coughing. The best "cough med" for a child with asthma is always the asthma medicine. Caution: don’t use cough suppressants. If over 6 years old, cough drops may help a tickly cough.
- Caution: If the inhaler hasn’t been used in over 7 days, prime it. Test spray it twice into the air before using it for treatment. Also, do this if it is new.
- Use the medicine until your child has not wheezed or coughed for 48 hours.
- Spacer. Always use inhalers with a spacer. It will get twice the amount of medicine into the lungs.
- Asthma Controller Medicine:
- Your child may have been told to use a controller drug. An example is an inhaled steroid.
- During asthma attacks, keep giving this medicine to your child as ordered.
- Allergy Medicine for Hay Fever:
- For signs of nasal allergies hay fever, it’s okay to give allergy medicine. Reason: Poor control of nasal allergies makes asthma worse.
- Fluids – Offer More:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- Reason: It will loosen up any phlegm in the lungs. Then it’s easier to cough up.
- Humidifier:
- If the air in your home is dry, use a humidifier. Reason: Dry air makes coughs worse.
- Avoid Tobacco Smoke:
- Tobacco smoke makes asthma much worse.
- Don’t let anyone smoke around your child.
- Avoid or Remove Triggers:
- Shower to remove pollens or other allergens from the body and hair.
- Avoid known causes of asthma attacks such as smoke or cats.
- Do not take part in sports during the attack.
- What to Expect:
- If treatment is started early, most asthma attacks are quickly brought under control.
- All wheezing should be gone by 5 days.
- Inhaler With a Spacer: How to Use
- Step 1. Shake the inhaler well. Then attach it to the spacer holding chamber.
- Step 2. Breathe out completely and empty the lungs.
- Step 3. Place the mouthpiece of the spacer in the mouth.
- Step 4. Press down on the inhaler. This will put one puff of the medicine in the spacer.
- Step 5. Breathe in slowly for 5 seconds until the lungs are full.
- Step 6. Hold a deep breath for 10 seconds. Allow the medicine to work deep in the lungs.
- If your doctor has ordered 2 or more puffs, wait 1 minute. Then repeat steps 2-6.
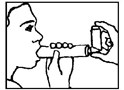
- Metered Dose Inhaler MDI: How to Use Without a Spacer
- Step 1. Shake the inhaler well.
- Step 2. Hold the inhaler about 1-2 inches 2-5 cm in front of the mouth.
- Step 3. Breathe out completely and empty the lungs.
- Step 4. Press down on the inhaler to release a puff. Do this just as your child starts to breathe in.
- Step 5. Breathe in slowly for 5 seconds until the lungs are full.
- Step 6. Hold a deep breath for 10 seconds. Allow the medicine to work deep in the lungs.
- If your doctor has ordered 2 or more puffs, wait 1 minute. Then repeat steps 2-6.
- Ask your doctor for a spacer. It will help send more medicine into the lungs.
- Home Nebulizer: How to Use:
- A nebulizer machine changes a liquid medicine med into a fine mist. The fine mist can carry the med deep into the lungs. This is called a nebulizer neb treatment.
- Step 1. Prepare the medicine. First, wash your hands with soap and water. For pre-mixed single dose vials, just add one vial to the neb holding cup. For multi-dose vials, you need to do the mixing. First, add the correct amount of normal saline to the neb cup. Then carefully measure and add the correct amount of medicine to the saline.
- Step 2. Connect the nebulizer to the air compressor tubing. The air compressor is run by electricity. Portable ones run on a battery. Compressors make the jet of air that turns the medicine into a fine mist.
- Step 3. Turn on the air compressor. It will start making the fine mist that your child needs.
- Step 4 for an Older Child. Place the mouthpiece between your child’s teeth and seal with the lips. Ask your child to breathe slowly and deeply. Ask your child to hold a deep breath for 10 seconds once a minute.
- Step 4 for a Younger Child. If your child refuses the mouthpiece, use a face mask. It should cover the nose and mouth. It should fit snugly.
- Step 5. Continue the treatment until the med is gone. If the med sticks to the side of the cup, shake it a little. An average neb treatment takes 10 minutes.
- Step 6. After each treatment, take the nebulizer apart. Rinse and clean it as directed. Reason: It can’t produce mist if it becomes clogged up.
- Caution: Closely follow your doctor’s instructions. Use the exact amount of med your doctor ordered. Don’t give a neb treatment more often than every 4 hours.
- Call Your Doctor If:
- Trouble breathing occurs
- Asthma quick-relief medicine neb or inhaler is needed more than every 4 hours
- Wheezing lasts over 24 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the ‘Call Your Doctor’ symptoms.
Disclaimer: This information is not intended be a substitute for professional medical advice. It is provided for educational purposes only. You assume full responsibility for how you choose to use this information.
Copyright 1994-2015 Barton D. Schmitt, MD. All rights reserved.
“Dr Aughney is the best. Very good with both kids and parents. My kids never have a fear to go and see him because they trust him which is so important.”
“Our family has gone to the Pediatric Center for decades. We have always been treated well by the friendly, knowledgeable staff. We love Dr. Anderson and Dr. Edwards especially, but all the doctors and nurses are fantastic! They are each compassionate and trustworthy. We recommend everyone to the Pediatric Center.“
“We love the pediatric center! Everyone is always so helpful and every physician we have seen answers all our questions and makes us feel confident in taking care of our baby!“