All About Allergies!
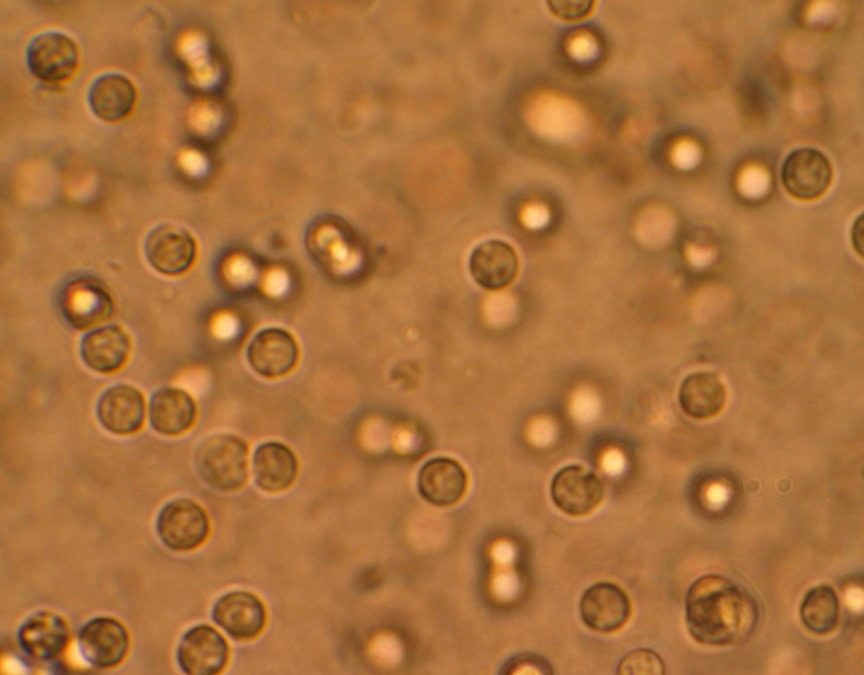
Everyone is excited about spring with the warmer temperatures and sunshine it can bring! However, for those that struggle with allergies, the increased pollens in the air can cause miserable allergy symptoms. Nasal allergies are an allergic reaction of the nose and sinuses to an inhaled substance. Most allergens float in the air. Trees, grass, weeds, and mold are the most common pollens. Tree pollens come in the spring, grass pollens come in the summer, and weed pollens come in the fall. Most nasal allergies continue through pollen season and can last 4 to 8 weeks.
Seasonal pollen allergies usually begin around 2 to 5 years and peak in school-aged children, teens, and young adults. Pollen symptoms are rare in children under 2 since they require at least 2 seasons of exposure to the pollen. If a child under 2 has chronic nasal symptoms, it is most likely due to other causes such as recurrent colds, large adenoids, or a cow’s milk allergy. Fevers do not accompany nasal allergies.
SYMPTOMS OF NASAL ALLERGIES
- Clear nasal discharge with sneezing, sniffing, and itching of the nose
- Red, watery, itchy, and puffy eyes
- Ear and sinus congestion or fullness
- Scratchy, hoarse, or tickly throat
- Itchy ear canals or skin
- Symptoms occur during pollen season
- Similar symptoms occur during the same month of the last year
TIPS TO HELP WITH NASAL ALLERGIES
Have your child shower before bedtime to remove the pollen from the hair and skin. Keep windows closed in the home and the car, and turn on the air conditioner in your car to recirculate to help. Try to avoid window or attic fans which can pull in pollen. It is also helpful to stay indoors on windy days because pollen counts are much higher when it is dry and windy! Last, avoid playing with outdoor dogs, pollen collects in their fur.
MEDICATION FOR ALLERGIES
The key to controlling allergies is to give allergy medication every day during pollen season.
- Allergy medicines are called antihistamines. They are the drug of choice for nasal allergies to help control symptoms such as runny nose, nasal itching, and sneezing.
- You can give a short-acting allergy over-the-counter medicine such as Benadryl every 6-8 hours.
- The bedtime dosage is especially important for healing the lining of the nose.
- You can also use a long-acting over-the-counter allergy medicine such as Zyrtec. This medicine usually lasts up to 24 hours and may cause less drowsiness than Benadryl.
NASAL WASHES TO WASH OUT POLLEN
Saline nose drops or spray can help with seasonal allergies and are available at any drugstore without a prescription. This treatment helps to wash out pollen or to loosen up dried mucus. Put 3 drops in each nostril, blow each nostril out while closing off the other nostril, then repeat on the other side. Repeat nose drops and blowing until the discharge is clear.
Use nasal washes when your child can’t breathe through the nose or their nose is very itchy. Saline nose drops can also be made at home. Use ½ teaspoon of table salt, and stir the salt into 1 cup (8 ounces) of warm distilled or boiled water. A warm shower can also be effective to loosen mucus. Have your child breathe in the moist air, then blow each nostril.
If your child’s symptoms are not better in 2 days after starting an allergy medicine, contact the Pediatric Center for an appointment. At the Pediatric Center, we want to give you and your child the best information and treatment you can get. If your child becomes worse or you are concerned about your child’s health for any reason, please don’t hesitate to call the Pediatric Center. You can contact us at our Idaho Falls location at (208) 523-3060 or our Rigby location (208) 745-8927, to set up your appointment. We have a wonderful team of providers available for all of your children’s needs!